Drug-Resistant Fungi Adapt to Body Heat, Creating a 'Doomsday Scenario'
Drug-Resistant Fungi Adapt to Body Heat, Creating a 'Doomsday Scenario'
Drug-resistant fungi adapting to body heat is creating a concerning 'doomsday scenario' in the medical community.
Fungi, traditionally not as prominent as bacteria in discussions about antimicrobial resistance, are now becoming formidable threats. The adaptation of these fungi to the human body's internal temperature is particularly alarming because it enhances their ability to infect humans and evade current treatments.
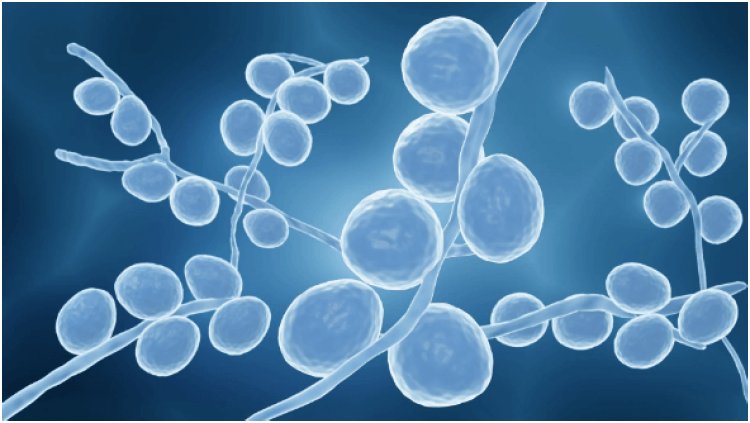
One of the most notable examples is Candida auris, a multi-drug-resistant fungus that has been causing outbreaks in healthcare facilities worldwide. C. auris is particularly concerning because it can survive on surfaces for extended periods, spreads easily between patients, and is resistant to multiple classes of antifungal medications. Its ability to thrive at human body temperature makes it a potent pathogen, capable of causing severe infections that are difficult to treat. Invasive infections, such as bloodstream infections, caused by C. auris can be fatal, especially in individuals with weakened immune systems.
The ability of fungi like C. auris to adapt to body heat is a significant evolutionary development. Most fungi thrive in environments cooler than the human body, which has historically acted as a natural barrier against fungal infections. However, with the increasing adaptability of these organisms to higher temperatures, this barrier is weakening. This shift is likely driven by climate change, which exposes fungi to warmer environments and prompts genetic adaptations that enable them to survive at higher temperatures. As a result, these heat-tolerant fungi are more likely to infect humans and other warm-blooded animals.
The implications of this development are profound. As fungi become more adept at surviving in the human body, they pose a greater risk to public health. The potential for widespread outbreaks of difficult-to-treat fungal infections is a significant concern. The medical community is already struggling with the rise of antibiotic-resistant bacteria, and the emergence of drug-resistant fungi adds another layer of complexity to the issue of antimicrobial resistance. The lack of effective antifungal treatments exacerbates this problem, as the pipeline for new antifungal drugs is limited compared to antibiotics.
Hospitals and healthcare facilities are at the forefront of this emerging threat. The environment in these settings can facilitate the spread of drug-resistant fungi, particularly among patients with compromised immune systems. Infection control measures, such as rigorous cleaning protocols and isolation of infected patients, are critical in preventing the spread of these pathogens. However, the resilience of drug-resistant fungi to standard disinfection methods makes this a challenging task.
Research and development of new antifungal therapies are urgently needed to combat the threat of drug-resistant fungi. Scientists are exploring various avenues, including the development of novel antifungal agents, combination therapies, and strategies to enhance the effectiveness of existing drugs. Additionally, understanding the mechanisms underlying fungal resistance and heat adaptation is crucial for developing targeted interventions. Advances in genomic and molecular biology techniques are aiding researchers in identifying potential targets for new antifungal drugs.
Public health strategies must also evolve to address the rising threat of drug-resistant fungi. Surveillance systems need to be strengthened to detect and monitor fungal infections, particularly in healthcare settings. Early detection and prompt treatment are essential in mitigating the impact of these infections. Public awareness campaigns can also play a role in educating healthcare professionals and the general public about the risks and prevention measures associated with fungal infections.
The role of environmental factors in the emergence and spread of drug-resistant fungi cannot be overlooked. Climate change, urbanization, and agricultural practices all influence the distribution and behavior of fungi. Efforts to mitigate climate change and manage environmental risks are integral to controlling the spread of these pathogens. Interdisciplinary collaboration between environmental scientists, microbiologists, and public health experts is necessary to develop comprehensive strategies that address the root causes of this issue.
The rise of drug-resistant fungi adapting to body heat presents a serious challenge to global health. The ability of these fungi to thrive at human body temperature and resist existing treatments creates a potential 'doomsday scenario' where fungal infections become increasingly difficult to manage. Combating this threat requires a multifaceted approach, including the development of new antifungal therapies, strengthening infection control measures, and addressing environmental factors that contribute to the spread of these pathogens.
The medical community, policymakers, and the public must work together to tackle this emerging crisis and prevent it from escalating into a widespread public health disaster.

 shivani
shivani